Peripheral Artery Disease (PAD)
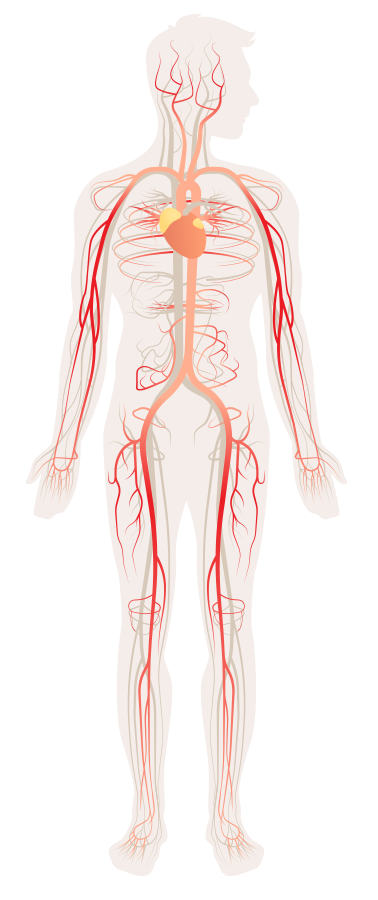
Plaque in the arteries of the trunk, arms, and legs can reduce blood flow to limbs and organs, causing pain, weakness, organ failure, and other complications. FreedomFlow® gives physicians a new, more flexible way to treat plaque blockages in the legs, from the small arteries in the ankle to the larger arteries in the hip.
One in three people over age 50 who have diabetes also have Peripheral Artery Disease (PAD)
What is peripheral artery disease?
Peripheral artery disease (PAD) refers to the build-up of plaque in the trunk, arms, and legs. This plaque reduces or blocks the flow of oxygen-rich blood, causing pain, weakness, and other complications.
PAD most commonly occurs in the lower abdomen and legs, but can affect arteries in the arms, kidneys, stomach, and head. Left untreated, it can lead to serious conditions such as stroke, organ failure, or—in the case of the leg—gangrene and amputation.
What are the symptoms of PAD in the lower extremities?
Typical symptoms include:
- Pain or cramping in the hip, thigh, or calf muscles—especially after exertion such as walking or climbing stairs
- Coldness, numbness, weakness, or heaviness in the leg
- Sores on the legs that won’t heal
- Weak pulse in the legs or feet
- Changes in skin color or shiny skin on the legs
- Erectile dysfunction in men
PAD prevalence in the US is on track to triple in the next 30 years
PAD usually occurs in people over the age of 70, although it can occur in younger people with risk factors such as obesity, diabetes, smoking, and high blood pressure.
Those with PAD are also more likely to have coronary artery disease or carotid artery disease—which can lead to heart attack or stroke.
How is PAD diagnosed?
Various tests may be used to diagnose PAD, such as:
- Tests to check the pulse and blood flow in the affected limbs – including an Ankle-Brachial Index (ABI), which compares blood pressure in the arms with that in the legs to see how well blood is flowing
- Blood tests – to check for diabetes and high cholesterol
- Treadmill test – to determine the impact of exercise on symptoms
- Ultrasound, MRI, or angiogram – to check the flow of blood through the affected area and look for blockages
What causes PAD?
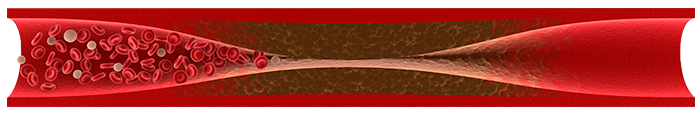
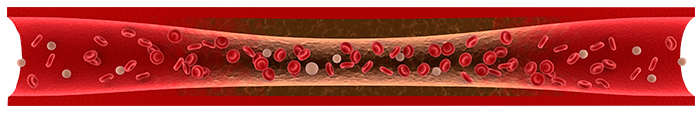
Atherosclerosis is caused by a build-up of plaque, which consists of fat, cholesterol, calcium, and fibrous substances in the blood.
Atherosclerosis appears to stem from damage to the walls of the arteries in the heart, which may be due to a combination of:
- High blood pressure
- High LDL (“bad”) cholesterol
- Low HDL (“good”) cholesterol
- Smoking
- Diabetes or insulin resistance
- Obesity
- Sedentary lifestyle
- Inflammation
Other factors—such as blood clots, physical injury, and genetic conditions—may also play a part.
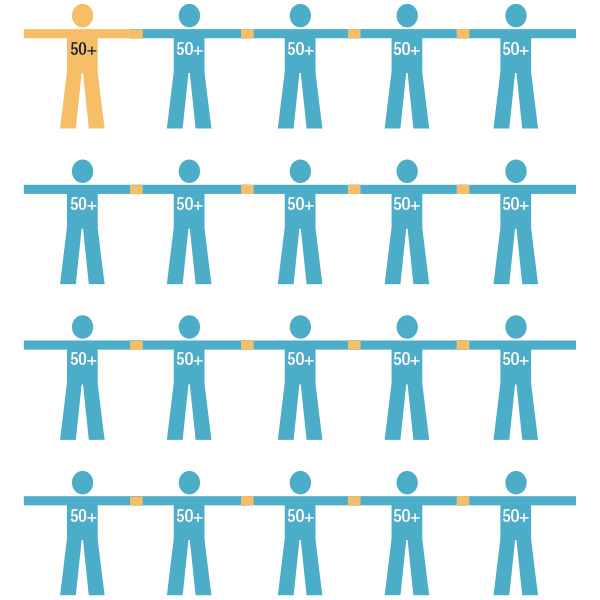
1 in 20 Americans over the age of 50 have PAD
How is PAD treated?
Those with less severe cases may be advised to make lifestyle changes through exercise, diet, and smoking cessation.
For more advanced cases, treatment may include:
- Medication – to reduce blood cholesterol or high blood pressure, prevent blood clots, or treat pain
- Angioplasty and stent placement – inserting a catheter into the blocked artery and inflating a balloon to press the plaque against the wall of the artery to improve blood flow; a stent (wire mesh tube) may be placed to keep the artery open
- Atherectomy – inserting a catheter into the blocked artery and using a special device, such as Cardio Flow’s FreedomFlow, to remove the blockage. It may be used prior to angioplasty and stenting if the plaque is especially hard to compress
- Bypass surgery – using a blood vessel from another part of the body to bypass the blockage
How many people are affected by PAD?
Nearly 8 million Americans are affected by PAD in the lower extremities, and the number is set to grow as the population ages due to the high incidences of diabetes, high blood pressure, smoking, obesity, and other risk factors in the population.
SOURCES: “Peripheral Artery Disease,” Mayo Clinic; “Peripheral Arterial Disease,” NIH: National Heart, Lung, and Blood Institute; Girish R. Mood, et. al., “Atherectomy in the Treatment of Lower-Extremity Peripheral Artery Disease: A Critical Review,” Vascular Disease Management, October 2013, 10:10), 192-197. All sources accessed online in December 2020.